
Reimbursement for care provided in the United States is based on productivity, i.e., work relative value units (wRVU), despite a shift towards value-based care by the Centers for Medicare and Medicaid Services.

These foci are crucial for healthcare quality, yet healthcare systems must also consider other factors. These performance dimensions can be applied to far-reaching, crucial healthcare challenges, such as reducing the massive rates of burnout present in healthcare workers and combating rising healthcare costs. The framework encompasses reducing costs, improving population health and patient experience, with a new fourth domain: healthcare team well-being. In 2014, the Quadruple Aim-adapted from the widely-accepted Triple Aim -was suggested as a framework to optimize healthcare system performance. The Creative Commons Public Domain Dedication waiver ( ) applies to the data made available in this article, unless otherwise stated in a credit line to the data. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. To motivate MAs, we engaged them to help with model improvements and showed gratitude for all the support they provide.Open AccessThis article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. Providers were motivated to improve these communication challenges because of the benefit of the additional staffing support. As a result, we adopted “in-room documentation” as our preferred terminology. MAs had strong negative reactions to being asked to “scribe,” as that role felt demeaning.

Quadruple aim for better administrative workflow full#
Providers struggled with allowing MAs the full time needed for the expanded rooming process, feeling the urgent need to begin the visit as soon as possible. The provider would then sigh in frustration, causing the MA to think she did her job incorrectly and then not elicit the full agenda with the next patient. For example, the MA would room the patient, elicit seven agenda items including an early refill on opiates, and relay the patient's agenda to the provider. Leadership noted early communication issues between providers and MAs. However, in implementing and sustaining these changes, we realized we had a lot to learn about provider-staff interaction and cultural issues affecting true team-based care. As a clinic providing integrated behavioral health care for more than 30 years, we thought of ourselves as team-based care experts. Work on communication issues (and don't call your MAs “scribes”). 5 Beyond reducing burnout, delivery models that rely on a high-functioning team have become essential given rapid increases in medical information and more prevalent chronic disease.
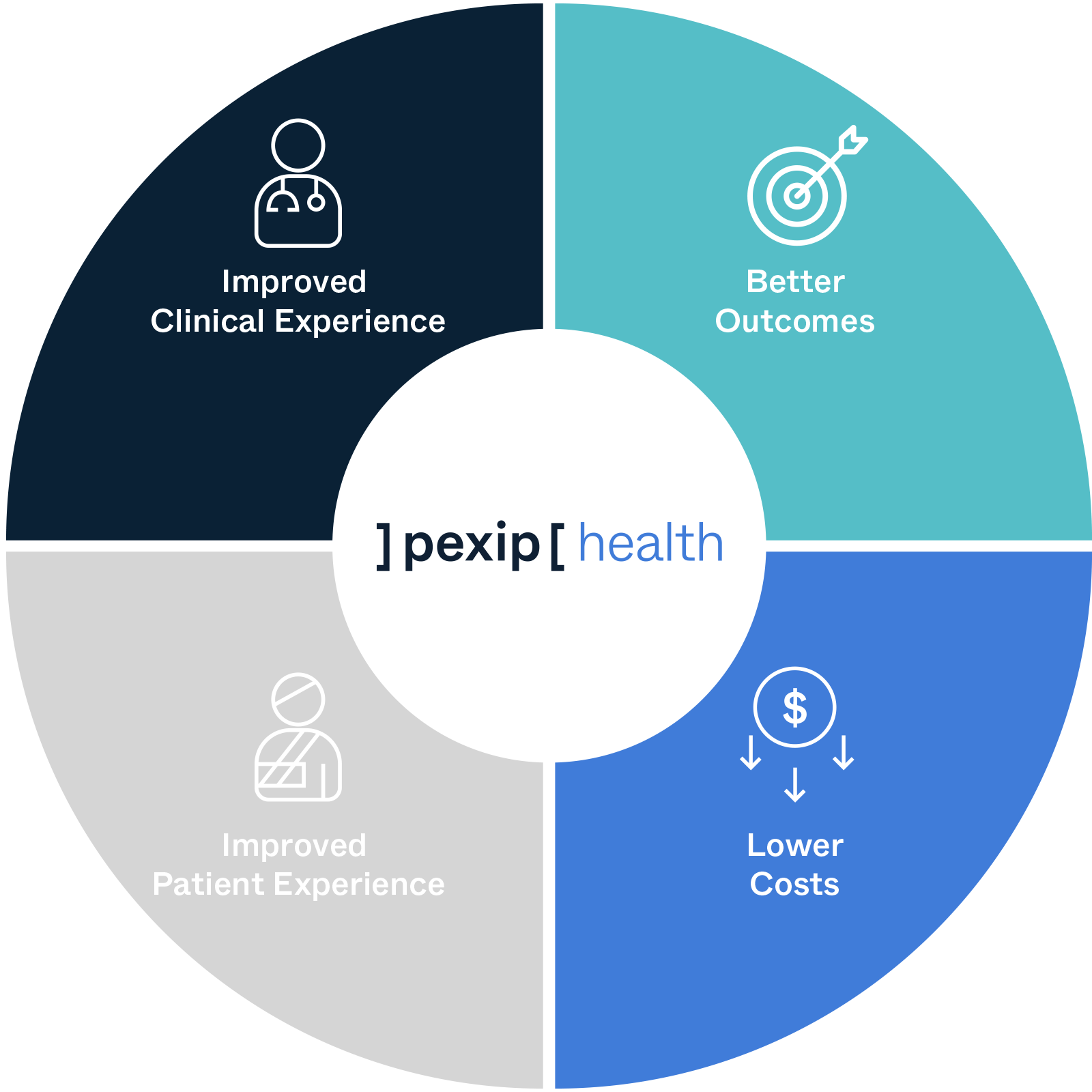
These strategies are designed not only to reduce provider burnout but also to reduce staff burnout by ensuring that they can grow professionally and engage more intimately in patient care. To achieve the Quadruple Aim, leading primary care organizations are exploring advanced team-based strategies such as team-based documentation, previsit planning and testing, an expanded scope of practice for medical assistants (MAs) and nurses, team-based motivational interviewing and coaching, and delegation of certain elements of chronic disease care, preventive care, medication reconciliation, refills, and acute care to staff using standardized protocols. As a result of these pressures, the “Quadruple Aim,” which adds provider and staff satisfaction to the Triple Aim, has been proposed as a more sustainable approach to improving health care.


 0 kommentar(er)
0 kommentar(er)
